COVID-19 in East Africa: Trust in a time of crisis – enabling continuity of essential services within a missionary approach to development
Key learning themes
• Trust, built up over years of presence in a community, was an essential element in maintaining essential health services as the challenges of COVID-19 unfolded.
• In the early weeks of the crisis, donor flexibility was vital in allowing projects to pivot funds and activities towards responding to COVID-19, principally in safeguarding health workers from infection, so that essential services could continue.
• The provision of clear, objective, scientifically sound and, above all, consistent information to the community was key to maintaining trust in health facilities and their staff, ensuring that people continued to present to the facilities for essential services and engage with health-seeking behaviours.
• In the under-resourced rural areas of sub-Saharan Africa, primary health care facilities were at the forefront, in terms of confronting the COVID-19 crisis and continuing to provide basic essential services.
• The hiring of non-clinical staff to help with patient flows and the maintenance of IPC protocols enabled clinical staff to concentrate on health service delivery.
Missionary development work
Established in 2004, Misean Cara is an Irish and international faith-based missionary development organization, made up of 88 member organizations working with some of the most marginalized and vulnerable people in over 50 countries across the world. At times of humanitarian crisis, the trusted and long-term presence of this organization in affected communities has allowed for rapid, efficient and targeted responses.
Over the many generations of Irish missionary involvement across many countries, the provision of health care has been an area of particular focus. The long-term presence mentioned above is also a key feature: one of the clinics included in the research described in this Brief was set up in 1885 by the missionary congregation that is still there today.
The emergence of COVID-19 in early 2020 brought new challenges to the provision of health care in poor communities in East Africa. Uncertainty, fear and misinformation all conspired to exacerbate a scenario which countries across all regions and resource levels were finding difficult to manage.
Misean Cara member organizations involved in the delivery of health care at primary, secondary and tertiary levels struggled to come to grips with the challenges they were facing: people were not presenting for routine health services as the perception spread that health facilities were the source of this new, unknown illness; health workers felt vulnerable to infection; and, in some instances, measures brought in by the Government to inhibit the spread of the virus added to the sense of panic and fear. Member organizations appealed to Misean Cara’s head office in Ireland for assistance.
Misean Cara’s first response was to listen to what members were saying. It became clear that radical and rapid measures were necessary. Immediately, Misean Cara permitted all projects, and not only those involved directly in health care, to pivot activities and funds towards responding to the crisis.
In the specific cases of health care projects, the first priority was to protect health care workers themselves, so that the provision of services could continue, as far as possible. Personal protective equipment was procured and distributed, and water and sanitation supplies were provided.
The second step was the setting up of dispensary and triage points outside health facilities, to minimize the risk of COVID-19 infection being brought into the facilities. Over 80% of project health facilities supported by Misean Cara reported that triage and dispensary capacity became vital to ensuring the continuity of services.
The third step was the training of health care workers in the symptoms and transmission modes of COVID-19. With this support, health care workers were more confident in managing patients presenting to their facilities.
Trust in a time of crisis
In July 2022, Misean Cara contracted the Royal College of Surgeons in Ireland to do research into how seven health facilities in East Africa (six in Kenya and one in Tanzania) responded during COVID-19. The research looked at two principal topics: how the facilities dealt with the pandemic, and how the provision of essential health services was impacted during that time.
The research found that trust – in health facility personnel, in the care provided as well as in the messages coming from the facility – was a key element in encouraging people to return for essential services. This trust had been built up over many years of engagement by missionaries who were clearly committed to improving the health of the host communities.
During the uncertainties of the COVID-19 pandemic, one of the factors sustaining that trust was the careful communication of clear, scientifically sound and consistent information by the health facilities to the wider community.
Positive spill-over effects from the facilities’ direct COVID-19 response, such as enhanced WASH practices and better adherence to infection prevention and control measures, saw a reduction in other communicable diseases and more encouragement of health-seeking behaviours, encouraging attendance at health facilities, which were still operational. Misean Cara funding (provided through four funding rounds) was targeting COVID-19 responses, which enabled facilities to fill gaps and scale up its COVID-19 strategy without the need to reallocate internal resources at the cost of other services.
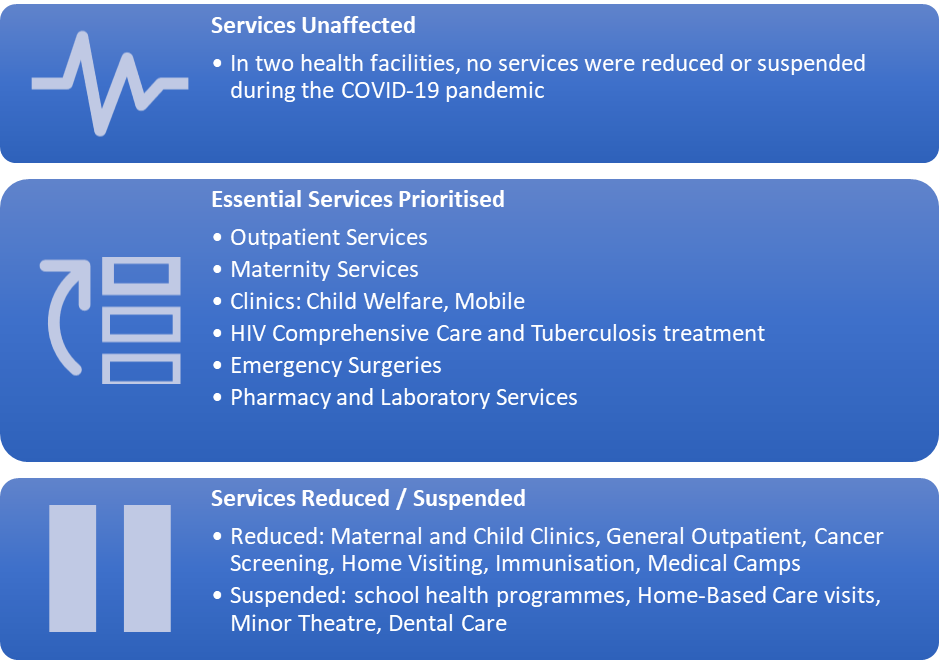
Despite national restrictions, and initial disruptions to outreach activities, all health facilities in the sample managed to maintain essential health services during the pandemic, some with adaptations.
Using the WHO Operational Guidance for the COVID-19 Context, the health facilities addressed the challenges as follows:
• Decisions were made to prioritize essential services (outpatient, maternity, child welfare, HIV & TB treatment, emergency surgery), while temporarily suspending outreach programmes and non-urgent services, such as minor surgery and dental care.
• Within the facilities, contacts were limited and safe patient and staff flows established, frequently with the assistance of non-medical staff.
• Some facilities established informal collaborations with nearby health facilities to share resources for their mutual benefit and the benefit of patients.
• Quick responses ensured the safety of front-line workers, with few (5.5% of clinical staff across the seven facilities) contracting or suspected of having caught COVID-19 infection.
Disclaimer
These HLH action briefs and learning briefs are presented for learning purposes only. Their content has been developed by the organization and author(s) named and as such does not necessarily represent the policies or approaches of WHO


