Post-conflict health system recovery efforts in South Sudan
Author
Moses Ongom1 , Oladipo Sotimehin1 , Sohel Saikat2 , Redda Seifeldin2 , Saqif Mustafa2
Author affiliations:
1. WHO South Sudan Country Office
2. WHO headquarters
The authors developed this case study in the context of a project on health system strengthening by building primary health care (PHC) foundations in South Sudan.
Country
South Sudan
Background
Since 2018, after five years of war, South Sudan is in a phase of transition, as its Government moves from a core focus of tackling a humanitarian and emergency situation towards reorienting the country’s priorities to long-term development of the health sector and provision and maintenance of essential health services. South Sudan’s health system performance has been significantly affected by the cumulative effects of protracted conflicts which have left millions in need of humanitarian assistance. The war destroyed both physical and social infrastructure, including the health system, resulting in very limited access and coverage of essential health services for the most vulnerable. For example, only 44% of the population live within a 5km radius of a health facility and only 68% of health facilities are functional.
Approach
With WHO’s three-level joint support to South Sudan, a plan for investments in catalytic actions to foster the recovery, growth and performance of the health system and services - the Health Sector Stabilization and Recovery Plan (HSSRP) - was developed for the period 2020-2022. This, however, coincided with the COVID-19 pandemic as it unfolded. The HSSRP aims to strengthen oversight and coordination mechanisms, performance monitoring systems and to improve the predictability of funding, as well as the sustainability and maintenance of essential health services. The plan also aims to enhance stewardship and accountability between humanitarian and development programmes.
Following this collaboration with the Ministry of Health and in-country partners, to develop the South Sudan HSSRP, the Ministry of Health was supported in its implementation of a health system strengthening project focusing on primary health care (PHC) in four states (Jonglei, Western Bahr el Ghazal, Eastern Equatoria and Central Equatoria). The project aimed to address some critical gaps in the health system’s foundations, including integration of health systems strengthening, emergency preparedness and response, and essential health service delivery efforts. It emphasized equitable health service delivery to vulnerable groups, particularly women and girls. It is also contributing to strengthening the country’s capacity for early warning, risk reduction and effective management of public health risks. The activities conducted supported South Sudan in efforts towards maintaining essential health services and early recovery in the midst of the unfolding COVID-19 pandemic.

Impact
The project strengthened national stewardship and partner coordination by facilitating the revitalization of the Health Sector Working Group and the establishment, scale-up and sustainability of the Health Sector Coordination Secretariat. This resulted in improved stakeholder engagement and coordination, which then enabled further action on HSSRP. The health development partners and the UN H6 (UNFPA, UNICEF, UN Women, WHO, UNAIDS, and the World Bank Group) technical and heads of agencies fora were revitalized as well. Available management and supervisory tools were also revised for improving Ministry of Health leadership and governance, and accountability at both national and state levels.

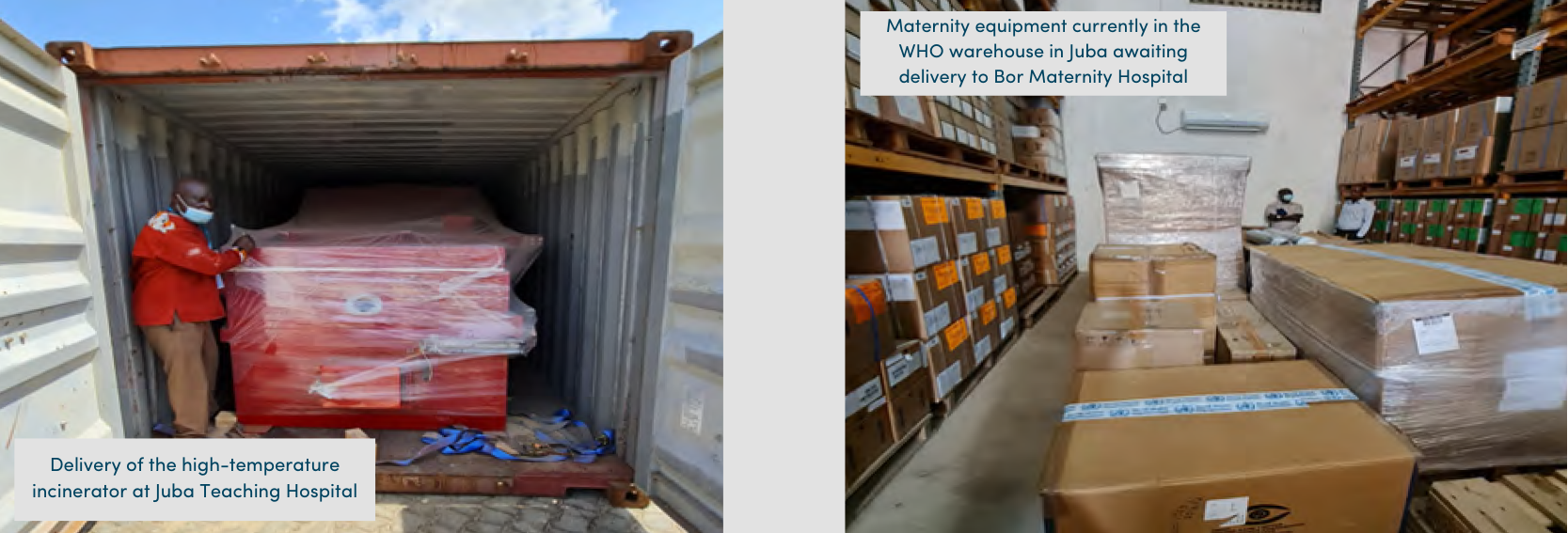
Major health facilities such as Juba Teaching Hospital (which also serves as the national tertiary/referral hospital) and Bor Maternity Centre (which serves a population of over 96 000 of the most vulnerable women and children) were rehabilitated, thus improving availability, quality and maintenance of essential health services. A high-temperature incinerator was installed at Juba Teaching Hospital, enhancing national capacity for infectious and hazardous waste management. The training of around 350 community resource personnel contributed to strengthening community-based surveillance of infectious diseases. Primary care was supported to improve the delivery of essential health services through procurement of core pipeline drugs for health facilities. To ensure longterm capacity development, the outdated curricula of all three university medical schools were revised to form one unified national competency-based medical training curriculum.
The project’s catalytic nature has also drawn additional support from donors and partners for health system strengthening and informed South Sudan’s progress in building PHC foundations as part of the first wave of Sustainable Development Goals Global Action Plan countries. Learnings emerging from this experience provide rich insights into how sustainable health system recovery can be achieved in conflict-affected contexts, with the adoption of a PHC approach, on the journey towards universal health coverage.


