The evolution of general practice accreditation in Australia to support primary care quality and patient safety
Disclaimer
Background and overview of the accreditation programme
The introduction of general practice accreditation in Australia in 1992 was influenced by several key publications and reports that highlighted the need for quality assurance and improvement in primary health care, including The Future of General Practices: A Strategy for the Nineties and Beyond.¹
The Australian Government Department of Health and Aged Care (known then as the Australian Government Department of Health, Housing and Community Services) (the Department) funded the Royal Australian College of General Practitioners (RACGP) to develop standards for general practices with the aim of enhancing the delivery of health services through a process of continuous quality improvement. The standards for general practice were developed based on the best available evidence from relevant studies or from level IV evidence (i.e. experts). The RACGP Entry Standards for General Practices were launched in 1996. In developing the Standards, the RACGP reviews and considers all comparable national and international standards, as well as the International Society for Quality in Health Care (ISQua) Standards.
The Australian General Practice Accreditation Limited (AGPAL) became the first organisation responsible for the accreditation of general practices in Australia in 1997, laying the foundation for ongoing quality improvement efforts in primary health care. AGPAL has achieved ISQua organisational accreditation since 2005 and ISQua Surveyor Training Programme accreditation since 2015.
Accreditation of general practices in Australia remains voluntary. Incentive mechanisms have been incrementally introduced by the Commonwealth Government to encourage participation in the accreditation programme. In 1998, the Practice Incentives Program (PIP) commenced with accreditation introduced as an eligibility criterion to the programme. The aim of the PIP was to provide financial incentive benefits to general practices to support the provision of quality care, enhance capacity and improve access and health outcomes for patients.
In 2019, the Practice Incentives Program Quality Improvement Incentive (PIP QI) was introduced, encouraging practices to participate in quality improvement activities, aimed at improving patient outcomes through the delivery of quality care. To participate in the PIP QI, practices must be accredited against the RACGP Standards for general practices.
In 2012, the financial incentives expanded to include the Practice Nurse Incentive Program (PNIP), now known as the Workforce Incentives Program (WIP), which is aimed to provide financial incentives to general practices that employ nurses, Aboriginal and Torres Strait Islander health workers and practitioners, and allied health professionals.
In January 2017, the Australian Commission on Safety and Quality in Healthcare (the Commission) partnered with the RACGP to develop a model accreditation scheme for general practices in Australia - the National General Practice Accreditation (NGPA) Scheme. This followed a recommendation from the Australian National Audit Office.²
The NGPA Scheme provides a governance framework for national coordination of general practice accreditation and an approval process for accrediting agencies. The NGPA Scheme sets out the responsibilities of accrediting agencies in relation to the implementation of the relevant safety and quality standards.³ There are currently four approved accreditation providers for general practice in Australia, of which AGPAL remains the market leader, accrediting approximately 5,000 general practices nationally.
In 2021, the Department commissioned an independent review of general practice accreditation arrangements, including the NGPA Scheme. The purpose of the consultation was to seek stakeholder feedback on the strengths and limitations of general practice accreditation and its intersection with educational accreditation.⁴
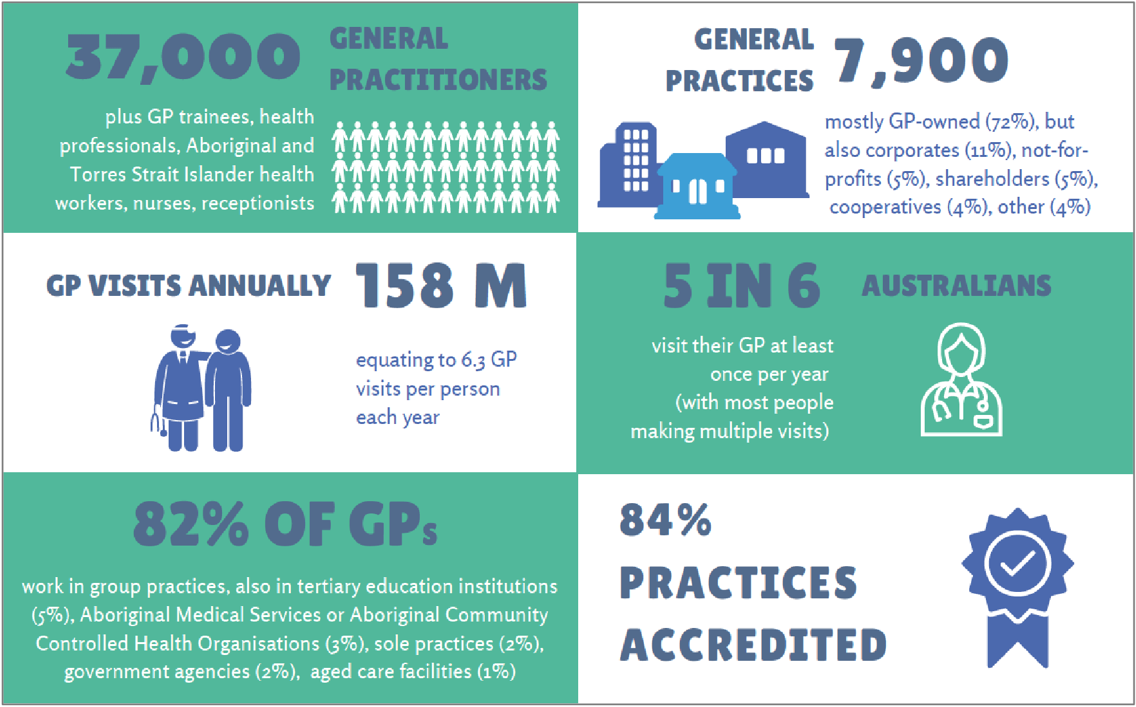
Diagram 1: Australian general practice key statistics⁵
¹ Commonwealth of Australia. The future of general practice: a strategy for the nineties and beyond. General Practice Consultative Committee, 1992.
² Australian National Audit Office (ANAO)
³ NGPA Scheme
⁴ Review of general practice accreditation arrangements
⁵ Data is drawn from: Australian Institute of Health and Welfare, July 2020, Australia’s health in 2020 – Primary health care; EY Sweeney, May 2020, RACGP GP Survey cited in the Royal Australian College of General Practitioners (RACGP), November 2020, Health of the Nation 2020; Medicare Benefits Schedule (MBS) data.
How was accreditation used to improve the quality of health services?
In Australia, general practitioners (GPs) provide a broad range of services to patients, including preventive care and the diagnosis and treatment of illness and injury, through direct service provision and/or referral to acute (hospital) or other health services. The service delivery model and nature of services are diverse and have become more person-centred over the years, using multi-disciplinary teams to deliver care. Accreditation is an integral part of safe and quality general practice in Australia. It is an independent recognition that practices meet the requirements of the governing national industry standards. Accreditation of general practice in Australia is not legislated, but it is influenced by health care policy.
The RACGP standards state that the purpose of quality improvement is for general practices to identify opportunities to make changes that will improve patient safety and care. Quality improvement can be achieved in a number of ways, one of which is the regular review of practice’s structures, systems and clinical care. Improvement needs to be based on the practice’s own information and data, which can be collected in a variety of ways, including feedback from patients and the practice’s team, and audits of clinical data. All members of the practice team need to have opportunities to contribute to the practice’s quality improvement activities⁶.

Source: Australian General Practice Accreditation Limited
Peer assessors, often GPs and other healthcare professionals, conduct on-site visits and evaluate the practice's adherence to the established standards. This assessment includes a review of policies, procedures, patient records, infection control measures, facilities, and governance structures.
The assessors provide feedback and recommendations to address any gaps or deficiencies identified during the assessment process; this feedback allows practices to implement necessary changes to enhance their services and meet the accreditation standards.
The assessment process broadly includes: a self-assessment completed by the practice; a desktop review of information provided by the practice; an on-site assessment at the practice; a report; and a remediation period for practices to address any non-conformances and submit evidence of conformity.
General practices are expected to maintain conformance with the standards throughout the accreditation period and engage in continuous quality improvement (CQI). There are CPD initiatives provided by RACGP to encourage and support practices to engage in CQI.
The standards for general practice accreditation have evolved over the years and now place a stronger emphasis on patient-centred care and safety and quality improvement.
Whilst accreditation of general practices in Australia remains voluntary, over 80% of general practices in Australia are accredited. The total is continuing to grow with more government payments to be linked to accreditation and the new My Medicare patient enrolment model Australia embraced in October 2023.
Here are some examples of varying general practices, an Aboriginal Torres Strait Islander Community Health Service, and Aboriginal community controlled regional health service sharing their experience of going through accreditation:
- Groveway Medical
- Camp Hill Healthcare
- Rosedale Medical Practice
- Aboriginal and Torres Strait Islander Community Health Service (ATSICHS)
- Maari Ma Aboriginal Health Corporation
Currently, many government initiatives and funding programmes require practices to be accredited to be eligible to participate. Accreditation is an eligibility criterion to access a number of Commonwealth programmes which collectively constitute between 6-12% of practice income depending upon location (rural practices are paid more) and the billing type of the practice (private billing practices apportion a smaller percentage of income to government payments).
The programs include the:
- PIP – The PIP comprises eight incentive payments under three payment streams – quality stream, capacity stream and rural support stream. MBS data shows that a total of $443 million, were made in PIP payments to 6 533 general practices in the 2020-21 financial year, indicating that on average each practice received $68 000 in PIP payments (noting there is significant variation in payment amounts depending on the size of the practice and the number of incentives in which the practice participates).⁷
- PIP QI – PIP QI payment is dependent on the size of the practice and is a maximum payment of $12,500 per quarter. Payments are based on $5.00 per Standardised Whole Patient Equivalent (SWPE), per annum to accredited practices who provide the PIP Eligible Data Set each quarter to their local Primary Health Network (PHN) and participate in continuous quality improvement activities in partnership with their PHN.⁸
- Workforce Incentive Program (WIP) Practice Stream – The WIP provides targeted financial incentives to encourage doctors to deliver services in rural and remote areas through the GP Stream and to employ practice nurses and allied health professionals through the practice stream. Over $387 million is paid annually to general practices and GPs through the WIP.⁹

Source: Australian General Practice Accreditation Limited
⁶ Royal Australian College of General Practitioners, Standards for general practice (5th edn), p. 8
⁷ Data provided by the Department of Health.
⁸ Royal Australian College of General Practitioners, Practice Incentives Program Quality Improvement Incentive (PIP QI) fact sheet.
⁹ For the period of 2019-20, see Services Australia, Annual Report 2019-20, p. 30.
What were the results of this activity?
The NGPA Scheme requires accrediting agencies to submit data on assessment outcomes to the Commission.
A summary of assessment outcomes and lessons learnt from the assessment of general practice can be found on the Commission’s website¹⁰ and highlights that, as at April 2023, 7,394 accreditation assessments had been conducted against the current (fifth edition) standards.
¹⁰ Assessment outcomes data and lessons learnt for the NGPA Scheme.
What were the key challenges involved? How were these challenges overcome?
Addressing the identified barrier or challenges and enhancing the value of Accreditation in primary health care
The journey toward accreditation in primary health care encounters some barriers and challenges that demand attention and resolution. This brief aims to elucidate some of these challenges while proposing strategies for overcoming them, thereby enhancing the value of accreditation within the global health community.
Perceived Discrepancy Between Costs and Benefits of Accreditation
A prevailing view within some healthcare sectors is that the financial and operational costs of accreditation may not proportionately reflect its benefits. This perspective often reduces the incentive for practices to pursue accreditation as a valuable endeavour, viewing it primarily as a prerequisite for certain financial incentives, such as Practice Incentive Payments (PIP), rather than as a significant quality improvement exercise. This outlook is particularly prevalent in settings with limited recognition of clinical excellence and leadership deficits.
- Strategies for Enhancement:
The Australian primary care reform agenda¹¹ presents a unique opportunity for us, to invest in enhancing clinical governance, leadership, and practice teams. Such investments are crucial for broadening the acceptance and integration of quality improvement protocols and care standardization. Furthermore, the purpose and benefits of accreditation must be clearly articulated and communicated to all stakeholders, emphasizing its role in continuous quality improvement. Accreditation should be perceived not as an intermittent requirement but as a continuous, integral practice within general healthcare operations, encouraging ongoing engagement rather than periodic compliance.
Strengthen Leadership and Engagement in the Accreditation Process
There is sometimes a lack of leadership and engagement by General Practitioners (GPs) in the accreditation process, with an overreliance on practice managers to navigate and fulfil accreditation standards.
- Strategies for Enhancement:
Enhancing the perceived value of accreditation among general practices, GPs, other health professionals, and patients is imperative. Additionally, providing targeted training and support to the practice team to develop and implement systems aligned with accreditation standards is essential. National health organizations, including the Royal Australian College of General Practitioners (RACGP), Australian College of Rural and Remote Medicine (ACRRM), and Primary Health Networks (PHNs), can play a pivotal role in encouraging and supporting practices to participate in accreditation. PHNs, in particular, could assist practices in system and process development to meet standards, aligning quality improvement activities with the accreditation journey.
Unique Challenges Faced by Rural and Remote Practices
Rural and, particularly, remote practices face unique challenges in applying accreditation standards due to the vastly different operational environments compared to their metropolitan counterparts.
- Strategies for Enhancement:
Future revisions of accreditation standards need to consider this and account for the diversity of practice environments, offering adaptability to meet the varied needs of all practices engaging in the accreditation process.
Scope and Focus of Accreditation Standards
The current scope, focus, and prescriptive nature of accreditation standards, including the extensive number of indicators, can impose a significant burden on practices to demonstrate compliance in a specific manner.
- Strategies for Enhancement:
Ongoing review and refinement of the standards are important. In Australia, the RACGP is currently reviewing the standards and working to ‘streamline the effort required by practices to meet the standards’ and is committed to continuously improve the standards to respond to ‘changes in the primary care landscape’. A continuous quality improvement approach to the standards will ensure they remain responsive to the evolving landscape of primary care. Focusing on outcomes offers practice teams greater ownership of their processes and systems, encouraging them to follow those processes not only during accreditation, but also before and after making it a permanent aspect of their operational ethos.¹²
In conclusion, addressing these barriers and challenges through strategic interventions and support mechanisms is essential for maximizing the value and impact of accreditation in primary health care. By doing so, we can enhance the quality and safety of patient care globally, in line with the World Health Organization's objectives for health system strengthening and improvement.
¹¹ Future focused primary health care: Australia’s primary health care 10 Year Plan 2022-2023.
¹² Preamble, RACGP Standards for general practices, 5th edition, pg. 3.
Key learning points
- The benchmark of the standards should continue to progressively elevate, whilst remaining achievable, with a continued focus on quality, safety, and alignment with governmental objectives for sector transformation and the delivery of more person centred, value-based care.
- Standards should cater not only to the exceptionally motivated but also offer avenues for all practices to excel. Incorporating health outcome measures or mid-cycle quality assurance activities could offer practices a rewarding way to exceed basic standards. Being able to differentiate practice achievement against more expansive standards could provide competitive advantages in patient care and staff recruitment.
- Streamlining indicators and avoiding overly prescriptive indicators will encourage practices to integrate documentation into a meaningful quality system, rather than for mere compliance with the standards. A gradual shift towards some outcome-focused indicators will enhance quality and patient safety.
- The general practice accreditation model should be a peer review process. This model fosters a culture of continuous improvement, safeguarding confidential information within a community of mutually interested parties, rather than external governmental entities
- To enhance the accreditation process, strategies and measures could be implemented or strengthened to improve the consistency between surveyors, decision makers and also between accreditation bodies.


