The role of compassion in maintaining quality essential health services during the COVID-19 pandemic
Background information
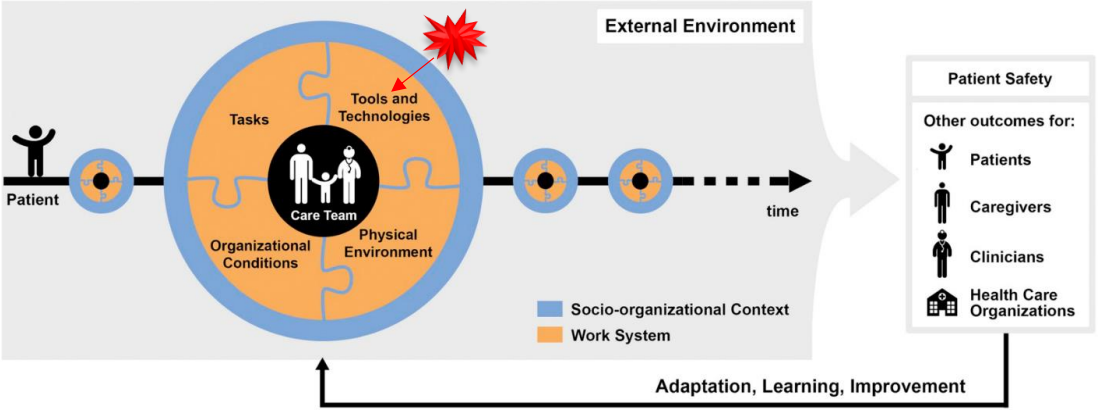
Role of the ergonomists/human factors
Two human factors (HF) engineers, in partnership with project management, were tasked by Materials Management and Infection Prevention to assess five potential replacement hand sanitizer stations. Changes in equipment design have potential for adjusting staff interactions. For a hand sanitizer station, changes in behavior may lead to less hand hygiene moments and possible hospital acquired infections. The individual assessments helped to define potential benefits and barriers prior to implementation for three end user groups (Nursing, Environmental Services, & Infection Prevention). HF engineers developed the methodology and design criteria, conducted assessments, compiled analysis and reports, and presented findings and recommendations to the stakeholders.
Main area of intervention
The hand sanitizer equipment (Tools & Technology) was changing due to the manufacturer discontinuing the model currently used throughout the hospital system.
A change in station design and sanitizing product (Tools & Technology) can be expected to have cascading effects on: Physicians and Nurses using the stations many times for a single patient encounter, Environmental services to stock and replace the cartridges (Care Team); the usage and replacement of cartridges (Tasks) ; the placement of stations, and storage of replacement cartridges on the unit (Physical Environment); the cost of purchasing from venders with and without previous business relations (Organizational); the number of hospital acquired infections due to hand hygiene compliance (Patient).
Aim of Patient Safety Project
Contracting Hospital: Carilion Clinic
Industry: Health Care and Quality & Patient Safety
Description
Method
The HF team conducted rapid assessments of five individual hand sanitizer stations, and provided information included in a report that highlighted initial impressions of the hand sanitizer stations. Insights were arranged into a Systems Engineering Initiative for Patient Safety (SEIPS) framework to categorize recommendations from the other user groups. The SEIPS framework assisted in identifying how the product design influences several factors for the context of use in a hospital setting. We modified questions from the SEIPS framework to help us evaluate each hand sanitization station:
- Does this tool\device used to perform the task of hand sanitization increase or decrease
the likelihood of safety events?-- - Ease of use
- Visibility of station and remaining product
- Ability to use safely without breaking
- Risk of creating a slip hazard with excess sanitizer pooling on floor - What in the physical environment can be sources of error or promote safety?
- Width of device may be too wide to fit in all existing hand sanitizer locations
- Color of sanitizer station is the same as the wall color
- What are the characteristics of the hand sanitization task in the person’s workflow that
could contribute to safe or unsafe patient care?
- The visibility of remaining product to know when to replace the cartridge
- Can only give sanitizer if pushed (i.e. unidirectional) there needs to be two stations for staff entering and leaving patients’ room to follow “foam in, foam out” policy - What are the characteristics of different persons performing the tasks or involved in the
work?
- Clinical staff constantly using hand sanitizer
▪ May lead to dry hands & disuse
▪ If the product leaves a film on hands it may be difficult to don and doff gloves
▪ Environmental services keep replacement cartridges on their carts
• If the weight of a replacement cartridge is too much there will be need to restock their work cart on multiple runs
Results
The distinct evaluation categories generated, helped present the benefi
ts and flaws of each hand sanitization station relevant to each end-user. The SEIPS framework helped the HF team identify nine criteria that were later used to help end-users evaluate these hand sanitizer stations. These criteria (shown in Table 1) were identified as themes and were found to be recurring patterns in our evaluations.
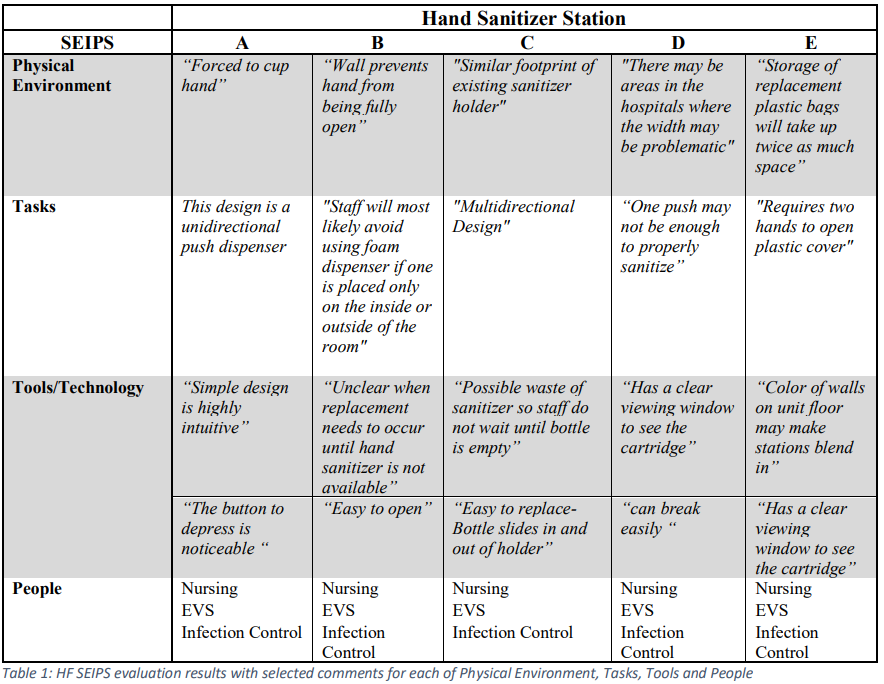
The nine evaluation criteria (Table 2) were then used to help multiple end-user groups choose between the five different hand sanitizer stations.
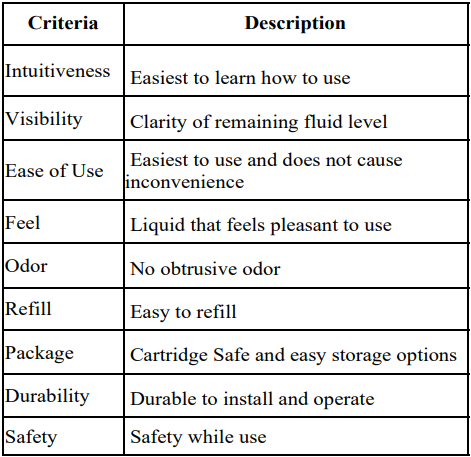
Table 2: Criteria generated through analyzing data through a SEIPS perspective
Thereafter, two types of survey forms (forced decision and priority ranking) were constructed to collect feedback from each end-user group, the responses were then transcribed by the HF team into a decision matrix.
Three groups: Nursing, Environmental Services and Infection Control used each sanitizer station (Figure 1) and then filled the survey forms.

Figure 1: Hand Sanitization Stations
Conclusion
Due to the SEIPS foundation to create the design criteria there were differences in the user groups design priorities as well as overall product preference. The results of the priority ranking in the first survey showed that Environmental services rated Visibility, Ease of Use, and Intuitiveness as their top three criteria. Infection prevention rated Safety, Ease of Use and Feel as their top three criteria, while Nursing rated Feel, Ease of Use and Odor as their top three criteria. Human Factors rated Safety, Durability and Feel as their top three criteria.
The results from the decision matrix scores generated from the surveys across all groups showed that out of all five sanitizer brands (A, B, C, D, and E), brand A was rated the best for infection control (score = 9.7), registered nurses (score = 7), and the human factors team (score = 9.8). The EVS team rated E highest (score = 11.8) followed by A.
Was the outcome evaluated following implementation?
Implementation of the new hand sanitizer brand is scheduled for early 2022. Existing hospital infrastructure is currently in place to monitor the implementation and use of the new product. Hospital safety event reports are tracked and monitored by Quality and Patient Safety team members; Infection Prevention has scheduled hand hygiene compliance checks and hospital acquired infection reports to gauge the success of implementing new hand sanitizer stations.


