.tmb-768v.png?Culture=en&sfvrsn=54737d84_1)
A large scale, rapid, virtual, support intervention for health care workers during the COVID-19 pandemic
Author
Dr Gareth Kantor - Faculty, Institute for Healthcare Improvement (IHI); Honorary Lecturer, University of Cape Town; Assistant Professor, Case Western Reserve University
Dr Beth Engelbrecht - Faculty, Institute for Healthcare Improvement (IHI); Adjunct Associate Professor, School of Public Health, University of Cape Town
Dr Pierre Barker - Chief Scientific Officer, Institute for Healthcare Improvement (IHI); Clinical Professor, University of North Carolina at Chapel Hill
Country
South Africa
Key Learning Themes
• Virtual collaborative learning spaces that are psychologically safe can be rapidly assembled to address workforce issues at a time of crisis.
• Adapt areas of focus to context – e.g. in South Africa, account for important role of unions power in the health care workforce.
• Senior level buy-in and endorsement.
• Seek partnerships for sustainability of work started in an emergency (e.g. Universities in health systems strengthening).
• Virtual designs may need to incorporate more traditional/formal network learning approaches (e.g. BTS) to transition from participatory learning to improvement actions, and improved outcomes.
What was the intervention or activity?
The aim of the intervention was to improve the ability of leaders (managers and clinicians) to provide physical and emotional protection to their health workers during the pandemic. The primary goal was to discover, borrow and develop effective strategies and tactics (local and global) that could assist leaders to achieve this aim.
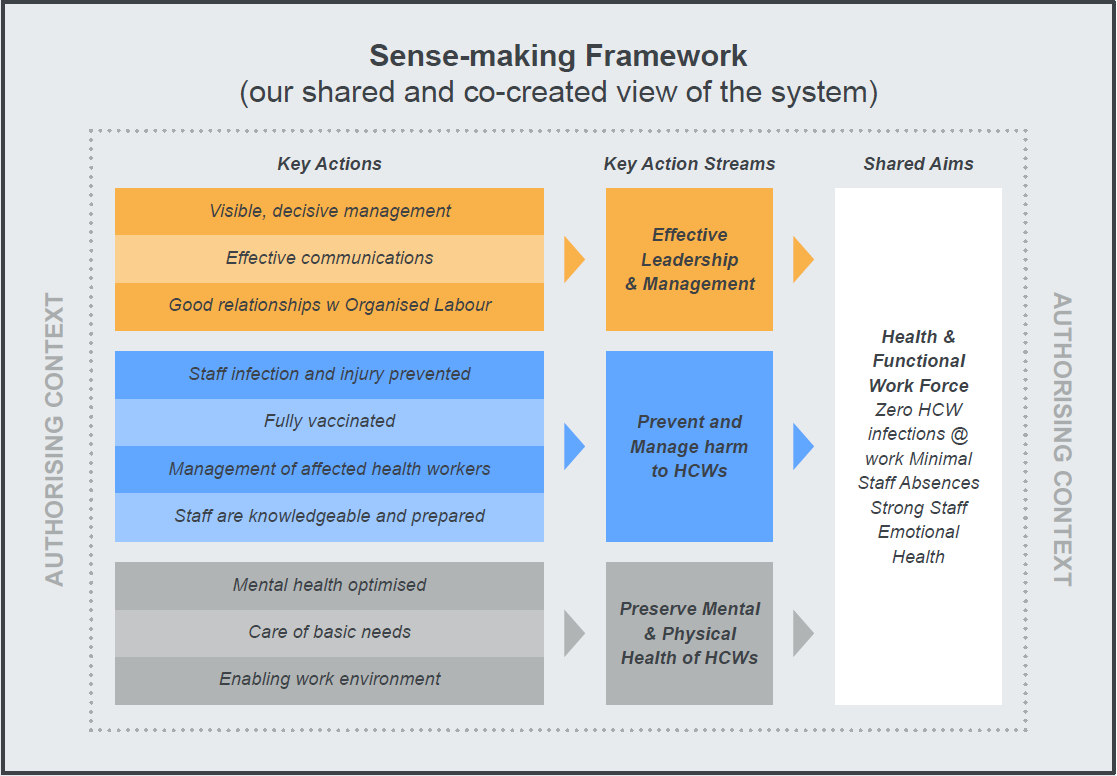
A “sense-making framework” (see the figure below) focused the activities of #StaffCare into 3 streams:
• Effective leadership communication and behaviours.
• Tactics and tools to protect health workers from COVID-19.
• Ways to support the well-being of workers during COVID-19.
The initiative introduced a number of evidence-based interventions and frameworks to guide the work of the initiative.
Following endorsement of #StaffCare by senior leadership (National Department of Health; Provincial Heads of Department), the initiative was implemented through 3 virtually enabled mechanisms:
• A steering committee in each province (high level health department leadership).
• A focus group (an “early adopter” group of mid-level leaders (managers and clinicians) meeting bi-weekly to share experiences and try out new ideas for change.
• CoLab group (a broader assembly of leaders (managers and clinicians) from across the provincial health system) that met every 4-6 weeks to learn from their peers.
The #StaffCare team supported specific activities: outreach to new provinces, convening of #StaffCare governance and learning communities, leadership and QI mentoring and coaching, development of supporting and sustaining partnerships, integration of #StaffCare into sustainable health system structures. Inclusion of the influential previous health system leadership in the #StaffCare team facilitated efforts to convene and spread the initiative to other provinces.
June 2021, version 3
Background
#StaffCare was initiated by IHI in May 2020 to support a South African Provincial Government's efforts to protect and support health workers during the COVID-19 pandemic. The initiative built off a national guideline that was issued to help protect health workers in the face of the COVID-19 pandemic and existing leadership training and virtual convening efforts by the Western Cape Department of Health (30,000 employees serving over 6m people).
In October 2020 #StaffCare established a partnership between IHI, provincial governments and other organizations (e.g. University of Cape Town, NMU) through a grant from the Rockefeller Foundation. The grant provided expanded support within the Western Cape Health Department and allowed scale up to two further provinces, North-West and Eastern Cape.
Impact of COVID-19 on essential health services
The pandemic disrupted routine services across the country. Elective surgery was cancelled and routine clinic visits were disrupted as resources and personnel were diverted to manage the pandemic. In the Western Cape, advance planning, expanded capacity, extended prescription periods for chronic conditions allowed most routine services to be maintained while the needs of the pandemic were addressed. In other provinces, there were major drop-offs in patient attendance for non-COVID conditions during the initial months of the pandemic that largely recovered within 12 months. The impact on some services such as child health services may be long term.
How did this intervention/activity contribute to the maintenance of EHS?
Staff well-being directly affects their ability to maintain essential and COVID-related health services during the pandemic. The impact of the pandemic on the well-being of the health system workforce, compounded a high prevalence of preexisting staff burnout. #StaffCare created inspiring, safe spaces that contributed to surfacing, testing, learning about and sharing specific ideas and tactics for leaders to improve staff well-being amidst the emotional pressure of COVID-19.
What were the key challenges involved? How were these challenges overcome?
• Endorsement of national and provincial leadership, but no clear mandate for leaders (managers and clinicians) to participate or expectation that they would undertake improvement work.
• Pre-existing punitive and blame cultures. Provinces other than WC lacked prior investment in distributed leadership principles, and an enabling organizational culture to adopt or easily participate in the learning structure offered by #StaffCare.
• Disrupted and distracted leadership in some provincial and national structures due to the burden of the epidemic and high turn-over rates.
• Exhausted workforce due to repeated waves of the pandemic.
• All-virtual interaction limited workshop opportunities to capacitate and plan action for method-naïve participants.
•Disruptive labour relations added to atmosphere of distrust between leadership and workers.
Mitigation Strategies:
• Build on, and establish trusting relationships.
• Demonstrate competence, accountability, empathy, a learning mindset approach.
• A partnership approach; meet teams where they are and not be prescriptive.
• A learning approach; establish a safe space for engagement.
• Leadership and improvement science mentoring though simple brief teaching modules suitable for virtual setting.
• Encourage leaders to “authorize” staff to test ideas and take action.
Please include any areas of support you require in the maintenance of essential health services
Health system strengthening through leadership, learning and improvement (QI) capability is core to ensuring employee wellbeing. A collaborative alliance of connected partners such as universities and NGOs can support public health and government systems. Strong macro and meso level governance capability is needed to maintain the focus on staff safety and wellbeing.


