.tmb-768v.png?Culture=en&sfvrsn=54737d84_1)
Strengthening Health Service Capacity: Harnessing data in response to the COVID-19 pandemic (Kenya experience)
Author
Country
Kenya
Introduction
Over the past 2 years, the COVID-19 pandemic has challenged public health systems and health services globally, revealing that even robust health systems can be rapidly overwhelmed and compromised by an outbreak. The disruption has been compounded by fear, stigma, misinformation and limitations on movement that hamper access to, and delivery of, health care services.
When health systems are overwhelmed, both direct mortality and morbidity from the outbreak and indirect mortality and morbidity from preventable and treatable conditions, increase.
At the start of the COVID-19 outbreak in Kenya, little was known about the capacity of health facilities to assure COVID-19 case management services or to maintain routine essential health services. What was the capacity of health facilities with regards to medical oxygen, ventilation, ICU beds, personal protective equipment, other IPC measures and trained staff? How were routine essential health services such as malaria, maternal health and deliveries, child vaccinations, hypertension, diabetes and cancer affected by the outbreak? What needed to be done to improve the outbreak response and control and limit disruption to essential health services?
This brief outlines actions and efforts by the Government of Kenya, in particular the Ministry of Health, to respond to the COVID-19 pandemic. It provides an overview of efforts to ensure the continuity of essential health services (EHS) and how this was informed by regular monitoring of the health facilities.
Response coordination structures
The Government of Kenya established the National COVID-19 Task Force and undertook a range of preventive and control measures to contain the COVID-19 outbreak, including enforced quarantines, lockdowns and curfews, as well as response measures strengthening and scaling the capacity of health facilities to provide COVID-19 case management.
In order to mitigate the adverse consequences on EHS, the MOH established a Technical Working Group on Continuity of EHS (CEHS-TWG) which provides guidance to the National COVID-19 Task force and the Ministry of Health Leadership.
Early on in the outbreak the CEHS-TWG developed national guidelines to support the continuity of essential services. Later these guidelines were aligned with the WHO Maintenance of EHS guidance. The guidelines defined priority EHS services and specified adaptations needed to keep people safe and maintain continuity of EHS during the response to the COVID-19 pandemic.
The TWG is responsible for identifying priority actions needed to maintain delivery of EHS during the pandemic and during the recovery and to advise healthcare managers on the provision of EHS.
Overview of efforts to ensure the continuity of essential health services (EHS)
Assessing and monitoring impact, disruptions and health system bottlenecks
To respond to the increasing demand for information on preparedness, the Ministry of Health established a system to monitor health service capacity through regular facility assessments and use of the routine health information system.
The objective of this health services surveillance system is to assess and monitor the readiness of facilities to provide the necessary and optimal care for suspected and confirmed COVID-19 patients, the extent to which essential health services are being offered and to identify health system bottlenecks. These assessments are being led by the Monitoring and Evaluation Division at the Ministry of Health. Findings are being used to inform policy makers and various stakeholders including Ministry of Health leadership, the National COVID-19 Task Force, the CEHS-TWG and development partners.
The COVID-19 health services surveillance system has been using both routine health information data monitoring sourcing the Kenyan Health Information System (KHIS) as well as regular health facility and community assessments. After the first round of facility assessments in June 2020 the MOH has been using the three WHO developed core assessment modules “Suite of health service capacity assessments in the context of the COVID-19 pandemic”. The three core tools are 1) Diagnostics, therapeutics, vaccine readiness, and other health products for COVID-19 - facility assessment tool, 2) Continuity of essential health services - facility assessment tool, and 3) Community needs, perceptions and demand - community assessment tool.
Two separate briefs on monitoring and assessments, one focusing on COVID-19 case management and a second one focusing on CEHS, describe in detail the processes, findings, challenges lessons learned and next steps of the respective assessment approaches.
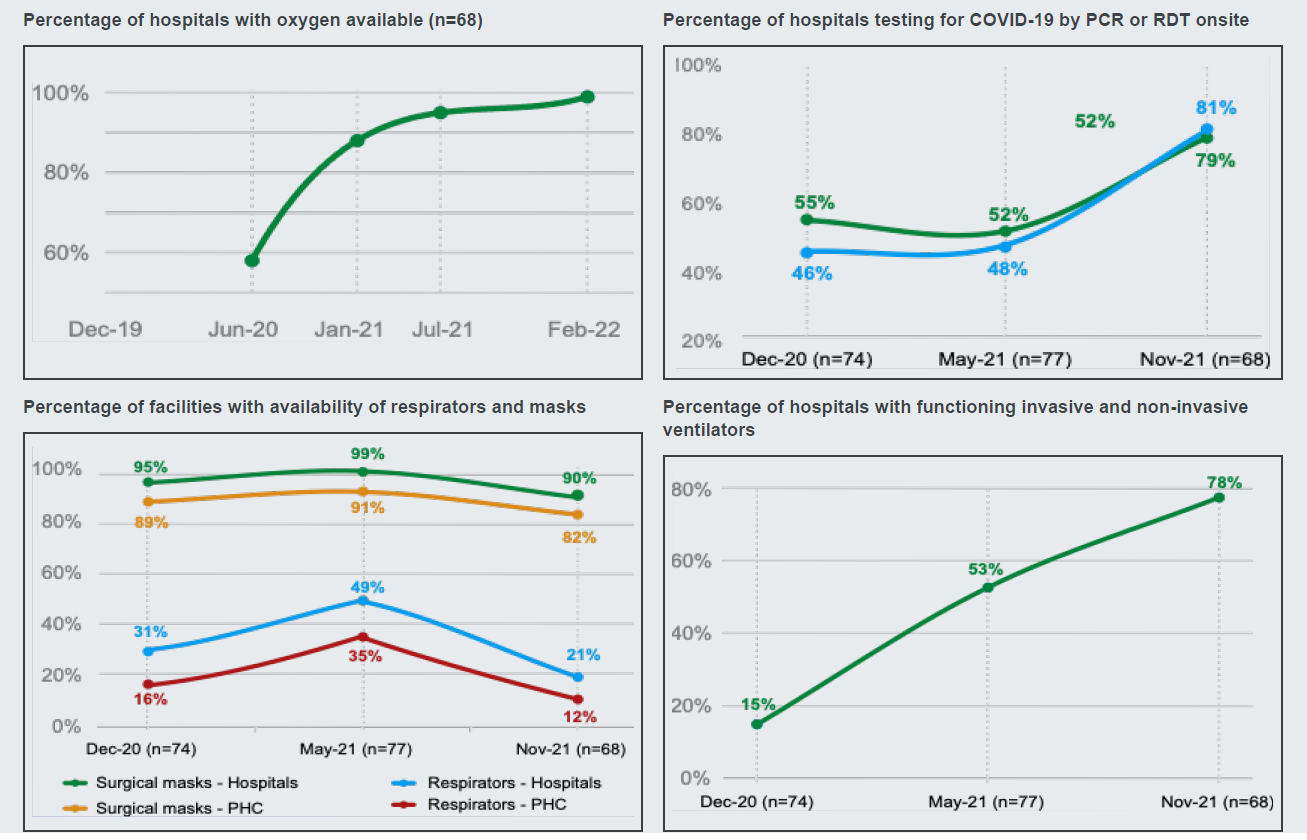
Main findings and informed actions with regards to COVID-19 case management
There were adequate beds available for non-critical COVID-19 cases (about 2,000 in 74 COVID-19 treatment centers) with a similar number available for conversion to COVID-19 beds in-case of a surge. Most of the assessed facilities had approximately 10% of their beds reserved for COVID-19 critical cases (ICU) with another 10% available. Oxygen was available in all COVID-19 treatment centers. Most facilities were using external oxygen cylinders which were reported to be quite expensive. Two of every three facilities had piped oxygen to the bedside, with ICU being the most common sites having piped oxygen.
• Ventilator numbers doubled in the assessed facilities between July and December 2020.
• Gaps were observed in availability of IPC guidelines, trainings on COVID-19 response and also readiness to provide COVID-19 vaccines among the facilities assessed. In terms of PPE, although most facilities had surgical masks for staff, many were lacking other equipment (i.e. clinical gowns).
• Testing for COVID-19 was accessible in most facilities but results took on average three days to receive.
• Drugs for treating COVID-19 were not adequately available in COVID-19 treatment centres. It was estimated that 10.4% of health workers had been diagnosed with COVID-19 in the past 3 months.
• Community health workers involved in managing COVID-19 did not feel adequately supported in their work.
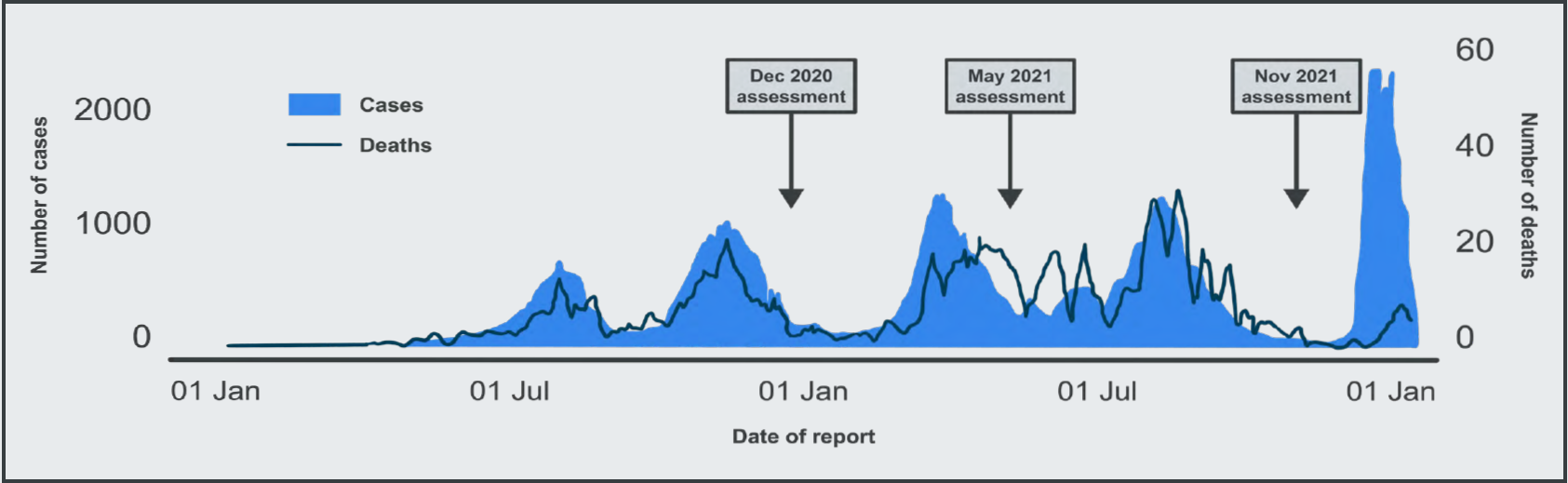
The graphics below show how regular assessment facilitates monitoring of health service capacity. Most assessed facilities significantly increased capacities to manage COVID-19 cases across the four assessment periods.
Main findings and informed actions with regards to maintaining priority EHS
Most services were negatively affected by the COVID-19 pandemic between 2019-2020, including utilization of general outpatient services for both adults and children, as well HIV and cancer screening services. This was mostly due to fear of contracting COVID-19 in health facilities. Maternal health services were more resilient and were only severely affected by a COVID-19 related health worker’s strike in December 2020. This strike had a negative effect on almost all indicators on essential services apart from cancer screening.
Counties with high number of COVID-19 cases were more affected with less patients visiting health facilities compared to those with a low number of cases. On a positive note, most indicators that showed poor performance early in the pandemic have shown good recovery as of February 2021.
Infection prevention measures were found to be sub optimal with all PPE items being available in only 4 in 10 of facilities assessed.
The tracking of EHS indicators in an integrated dashboard within the Kenya HIS facilitated the use of data for decision making. Providing structured feedback to facilities and Counties on a regular basis helped to ensure that supportive actions were rapidly undertaken.
This helped in planning for interventions such as home-based care, ensuring PPE access and PHC facility training. Many facilities put in place measures to mitigate these disruptions such as changing service hours, targeting high-risk patients, promoting self-care, telemedicine and combining care for multiple conditions into a single visit. Where it was noted that health facility utilization was low, communication materials were developed to inform citizens about available services.
Interventions carried out by other programs, such as expanding access to immunization services. Commitments were made by counties to support maintenance of EHS.
Lessons learned and next steps
Country driven assessments are key to the strengthening of health service capacity. Involvement of key stakeholders and rapid dissemination of findings is essential to ensuring that the findings inform policy and practice. An MOH EHS team that is comprised of different departments was key to the effective dissemination of assessment findings. Providing structured feedback to facilities and counties on a regular basis helped ensure supportive actions were rapidly undertaken. Methods to assess how the data has been used to inform decision making is important and needs further work.
The use of sentinel sites helped facilitate comparison between health facilities over time. The use of mobile phones was a safe, cost effective and efficient method of data collection within the context of COVID-19 restrictions. Key informant interviews at the national and county level will complement the quantitative findings from the facility assessments.
The use of multiple approaches to assess the continuity of EHS helped triangulate data and corroborate findings. Future rounds of data collection intend to involve a physical visit to facilities in order to verify findings.
The MOH will continue to monitor EHS based on routine KHIS data on a quarterly basis. This will inform sub-national approaches to maintain and strengthen service delivery and utilization. Impact assessments will be conducted periodically and as necessary to complement the routine reviews.
Adaptation to the evolving needs of the pandemic will be key to the implementation of these assessments.


